From up on our soapbox…
Medical imaging
Welcome to our new periodic series, where we get on our ‘soapbox’ to discuss some of the prevailing attitudes and practices in various aspects of healthcare, the evidence for or against and how it affects you.
We want to know what’s going on…
It’s understandable that, when a person feels pain, they want to know what’s going on. With musculoskeletal pain this can be difficult. When you have had some kind of trauma, (say, “rolled your ankle”, fallen off your bike or a car accident) there is often clear evidence of damage, like swelling, bruising or loss of function.
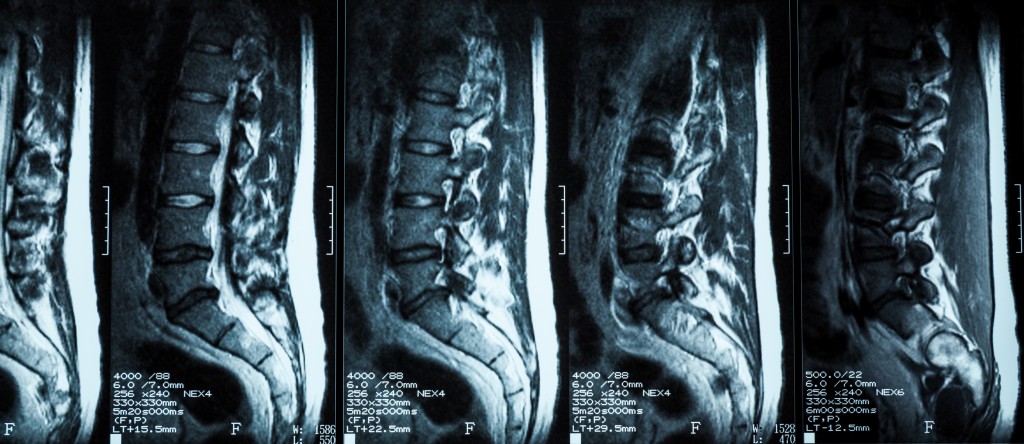
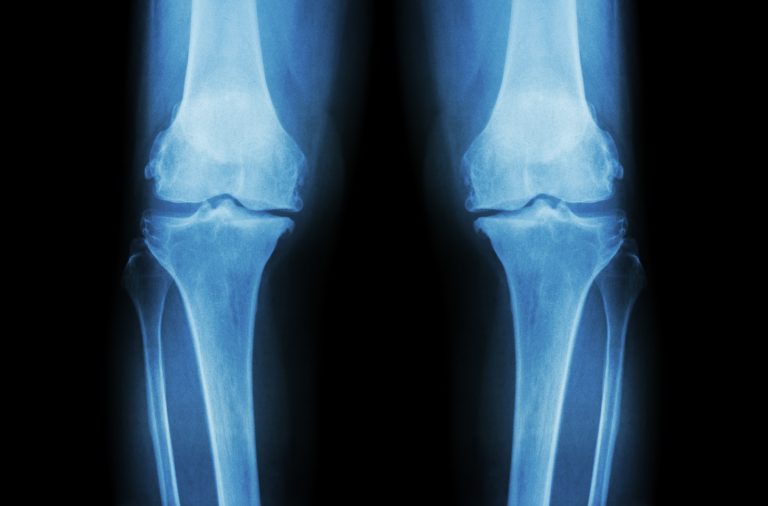
Many other causes of musculoskeletal pain, though, are not visible to the naked eye. For example, back, shoulder pain, neck pain and knee pain can be due to many tissues not visible to the naked eye (e.g bones, discs, tendons, ligaments, cartilage and nerves).
Imaging procedures using Xray, CT, ultrasound or MRI of internal tissues are often perceived to be the answer to damage not easily visible. These impressive technologies have steadily improved to the point where small internal structures are visible with these procedures.
What you see is not what you get…
Patients and practitioners need to consider using these technologies carefully because many studies have shown that pain does not correlate well with what’s seen on these images. For example, a Dutch MRI study of 194 patients who had experienced ankle trauma in the 12 months before the study found that “a substantial number of MRI abnormalities can be found in the contralateral (i.e. opposite and pain free) ankle” 1.
1 out of 7 participants had bone marrow swelling at the ankle of the pain-free foot and 1 out of 5 had abnormal findings in the pain-free foot of the ankle ligament that is often damaged in ankle sprains. Joint swelling was also present on MRI in the pain-free foot in 20% of participants.
A systematic review 2 of 3110 asymptomatic (pain-free) individuals whose lower backs had been imaged (by CT or MRI) showed that 37% of 20-year-olds showed signs of disc degeneration and 96% of 80-year-olds without low back pain showed signs of degeneration. Disc bulges were in seen in 30% of asymptomatic 20-year-olds and increased steadily to 84% of 80-year-olds.
Many other signs of spinal change thought to generate low back pain (disc protrusion, fissures, facet joint changes) were prevalent in pain-free individuals. The study also found that while vertebral slippage is not often seen in young people without pain, by the age of 60, it’s prevalence is 23% increasing to 50% in people without back pain in their 80s
This study also nicely summarises many studies of people in pain that show the degree of pain, the disability caused or the recovery outcomes are poorly correlated to the findings from imaging.
.
But what is really causing the pain?
If your practitioner is being honest with you, they would tell you that many causes of musculoskeletal pain are not clearly understood. This is why you may have heard the term “non-specific low back pain” if you have back pain; not because there is doubt the back pain exists but because the cause of the back pain is not clearly identifiable. An honest conversation with your practitioner needs to consider “how will this imaging procedure change my treatment plan?” If there will be no change to how you’re going to manage your pain, is it worth the cost in terms of time, money and depending on the procedure, exposure to radiation?
.
1 van Putte-Katier, N., Van Ochten, et.al., “Magnetic resonance imaging abnormalities after lateral ankle trauma in injured and contralateral ankles”, European Journal of Radiology 84 (2015) 2586-2592
2 Brinjikji, W., Leutmer, P.H., et. al., “Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations”, American Journal of Neuroradiology 36(4) (2015) 811-816